Hysteroscopy
Hysteroscopy
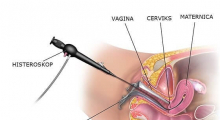
A hysteroscope is a special optical instrument of a small diameter (3-5mm).
What is hysteroscopy?
Hysteroscopy is a procedure of examining the interior of the uterus using an instrument called
hysteroscope. A hysteroscope is a special optical instrument with a small diameter of only 3-5mm, which is connected with a light source (for enlightening the interior of the uterus), a camera and a monitor.
Because of its small diameter, it is very easy to insert a hysteroscope into the uterus, which allows a
quality examination of the uterine cavity and abnormalities inside the uterus.
In most cases, the procedure is performed under a short-acting intravenous general anesthesia, and
lasts 10-20 minutes.
What are the benefits of hysteroscopy?
- Hysteroscopy is performed for both diagnosis of the uterine cavity conditions (diagnostic
hysteroscopy), and for treatments (operative hysteroscopy) when the detected abnormalities
are removed using the hysteroscope.
- Hysteroscopy has a very valuable role in the diagnosis of a number of gynecological problems:
- Infertility (in most IVF clinics hysteroscopy is a mandatory part of the preparation procedure
before the start of the very IVF process);
- Abnormal vaginal bleeding (excessive or irregular bleeding, bleeding between menstruation
periods, bleeding after sex, bleeding in the menopause);
- Unclear reasons for miscarriage;
- Presence of scar tissue inside the uterine cavity (intrauterine synechiae)
- Early stages of uterine mucosa cancer;
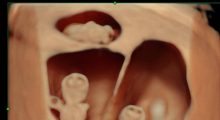
- Polyps or fibroids detected on other examinations (US, hysterosalpingography), as well as thickened mucosa or irregular shape of the uterus.
In a number of cases, hysteroscopy can be used as a treatment (a solution to the problem). For example, hysteroscopy can be used for removing the following from the uterine cavity:
- Submucosal fibroids (myomas that are in the inner layer of the uterus)
- Uterine mucosa polyps
- Uterine septum
- Intrauterine contraceptive device
- Scar tissue ( synechiae)
What do I need to know before the procedure?
Your doctor or a nurse will provide you with the information about the procedure. The procedure is
mostly performed in the operation room equipped with all the necessary instruments, and under a short-acting intravenous general anesthesia. For that reason, it is necessary to do some tests (preoperative preparation) prior to the procedure, so that we can reduce the potential and possible risks to the lowest.
The procedure is not done on the day you have a bleeding (as the blood can impair the view of the
uterine cavity). Before the hysteroscopy, make sure you are not pregnant. You will be advised on the
contraceptive methods which are to be followed from the first day of the cycle during which the
procedure is planned. If there is doubt, you need to do a pregnancy test.
After conversation with your doctor, you will get an informed consent to sign. This means:
- That you have got and understood all the necessary information about the procedure you are
about to undergo;
- That you agree to undergo the procedure.
How is hysteroscopy done?
At the scheduled time, following the previously received instructions, you come to the clinic.
You will have a short conversation with the doctors (anesthesiologist, gynecologist), and then
you will be transferred to the operation room. You will get drugs for general anesthesia (you will
sleep during the procedure).
Once you are under anesthesia, the doctor will surgically prepare the outer genitals and the
vagina in order to prevent any risk of infection, and then insert the hysteroscope through the
cervix into the uterine cavity.
If the endocervical passage is too narrow for the hysteroscope, a small instrument is used for a
permanent dilatation, so that the procedure can continue. The uterine walls are usually
“adhered”, so sterile saline solution is injected through the hysteroscope, which allows the
doctor to examine the uterine cavity.
During the intervention, a small portion of mucosa can be taken for histo-pathological analysis (endometrium biopsy). If a polyp or an adhesion is detected inside the cavity, a special instrument can be used for its removal. The whole procedure usually takes between 10 and 20 minutes.
What happens after the procedure?
After waking up in the operation room, you will be transferred into the patient’s room. You may feel
mild pain in the abdomen (like menstrual cramps). This is expected, but you may get some pain killers if you wish. After the procedure a light bleeding is possible, especially if a polyp was removed or a biopsy of the endometrium was done. You will stay in the patient’s room for several hours, until your condition is assessed before the discharge. Before leaving the hospital, the doctor will talk to you. If the procedure was performed under the general anesthesia (which is most often), somebody should take you home and stay with you for the next 24 hours. You are expected to be able to return to your normal activities later that day or the following day.
What should you pay attention to at home?
Vaginal bleeding and secretion. Light bleeding after the procedure is normal and can last 7-10 days. If
the bleeding is excessive (you have to change the sanitary napkin every 1-2 hours), or there are blood
clots, contact your doctor. Vaginal secretion may be excessive for up to 2 weeks after the procedure. If it becomes of a strong, bad smell, inform your doctor because it can be a sign of infection. In order to
reduce the risk of infection, during the period when the hysteroscopy was done use the napkins, not
tampons.
What are the side effects of anesthesia?
Every patient reacts differently to the anesthetic medicines, but side effects can include fatigue,
drowsiness, dizziness, nausea, and rarely vomiting. Organism takes 24-48 hours to clean itself from the anesthetic drugs. In this period rest is recommended with moderate daily activities.
When can I have sex?
Please, don’t have sex 5-7 days after the procedure, to reduce the risk of infection.
When can I have a shower or a bath?
You can have a shower on the same day, but wait for the bath until the day after the procedure. If you
still feel fatigue or dizzy, make sure somebody is at home with you.
What risks are connected with hysteroscopy?
Literally every medical procedure includes certain risks. The doctor will provide you with all the needed
information regarding potential risks and complications, before you get an informed consent to sign.
Complications are very rare and can occur during the procedure or after. Complications connected to
the anesthesia can also rarely occur.
Complications which occur during the procedure:
- cervix dilatation cannot be safely done- the procedure stops here;
- bad visualization (view) of the uterine cavity can affect the quality of information obtained with
hysteroscopy;
- perforation of the uterus with or without damaging other pelvic organs (this may require
additional surgery for damage reparation);
- excessive vaginal bleeding (this is a rare complication because the muscular uterine wall
contracts blood vessels that might be damaged during the procedure);
- Infection happens very rarely after the procedure. The procedure is done with sterile instruments, and in addition you get antibiotics. However, if one of these happens within 4-5 days after hysteroscopy, inform your doctor:
- vaginal secretion with bad smell;
- long-lasting excessive bleeding;
- severe abdominal pain;
- high body temperature (over 38°C);
- serious weakness.
Are there any alternative treatments?
There are alternative treatments, and they include: ultrasound, hysterosalpingography, dilatation and
curettage of the uterine cavity, etc. If an US examination for example detects a polyp, it can be removed by a dilatation or curettage. However, curettage is done without monitoring, so we cannot be sure whether the whole polyp was removed or just a part.
In general, there is no alternative method that allows such detailed information on the uterine cavity
like hysteroscopy. It not only enables the view of the abnormality, but also its removal. When the
endometrium biopsy is needed, hysteroscopy enables the “targeted biopsy”, the change the doctor
directly sees, and therefore gets the better result.
For all the aforementioned reasons, in modern day gynecology hysteroscopy is a golden standard for
diagnosis and treatments of the abnormalities in the uterine cavity.
Video gallery
Kako ukloniti polip iz materice? Histeroskopija - Dr Vilendečić Analife
Histeroskopija sa polipektomijom - dr Zoran Vilendečić - Analife
Gallery
Monday-Friday from 09-20h
Saturday from 09-15h
Opšta Bolnica Analife
Skadarska 5
(Zemun), Beograd